Published 27 November 2023
Say Goodbye to the Discomfort: Coping Strategies for Folliculitis
Understanding Folliculitis
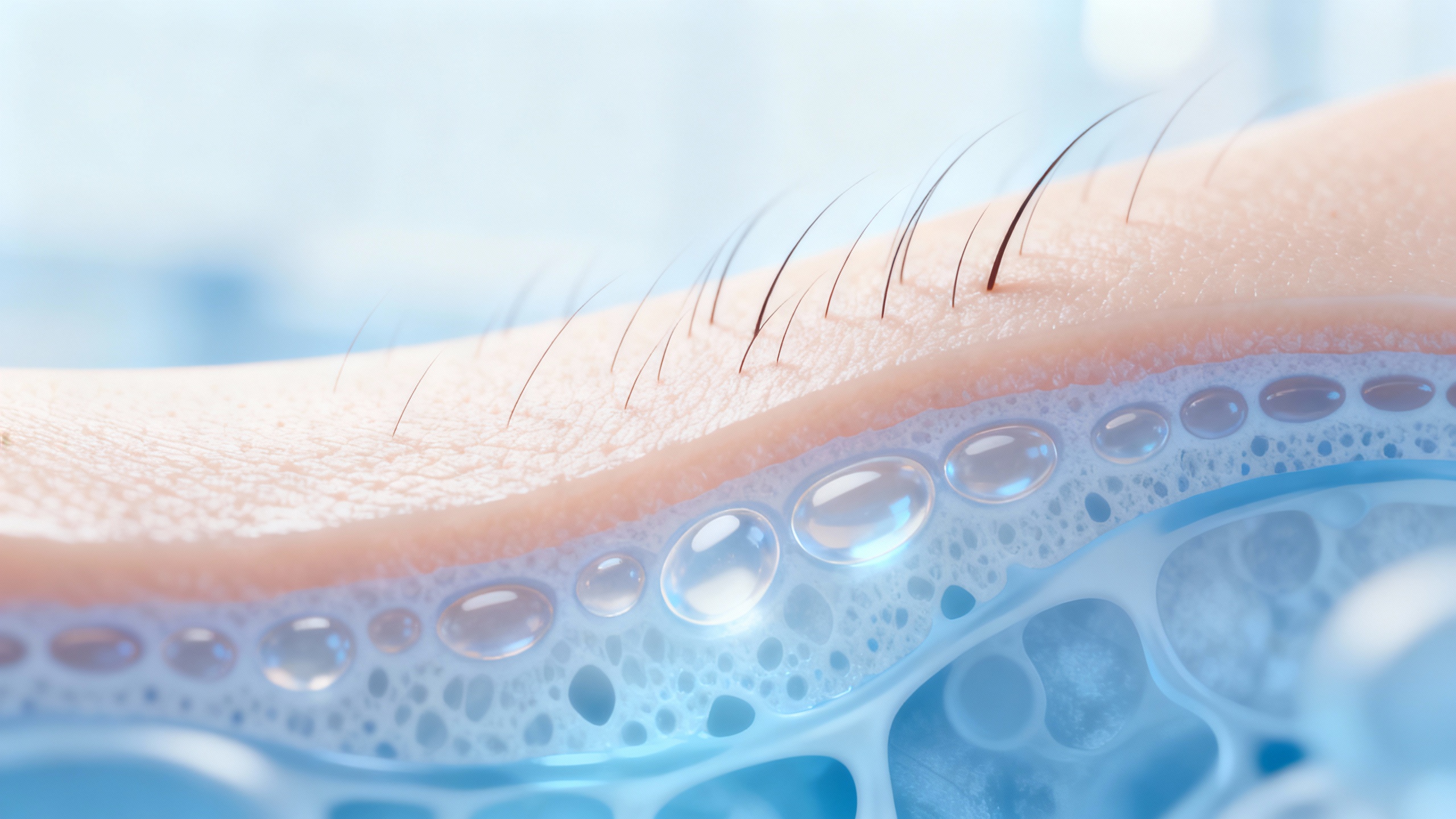
Folliculitis is a common condition that affects the hair follicles, causing inflammation and discomfort. It is important to have a clear understanding of what folliculitis is and its underlying causes and risk factors.
What is Folliculitis?
Folliculitis is a skin condition characterized by the inflammation of the hair follicles. Hair follicles are small openings in the skin from which hair grows. When these follicles become infected or irritated, it leads to the development of folliculitis. The condition can occur anywhere on the body where hair is present, including the scalp, face, neck, chest, back, and legs.
Folliculitis can manifest in various forms, including red bumps, pustules, or boils. These lesions may be itchy, painful, or tender to the touch. In some cases, folliculitis can resolve on its own without medical intervention. However, in more severe or persistent cases, medical treatment may be necessary.
Causes and Risk Factors
Folliculitis can be caused by various factors, including:
-
Bacterial Infection: The most common cause of folliculitis is a bacterial infection, often due to bacteria such as Staphylococcus aureus. These bacteria can enter the hair follicles through breaks in the skin, leading to infection and inflammation.
-
Fungal Infection: Fungal infections, such as those caused by yeast or mold, can also result in folliculitis. These infections are more common in warm and humid environments or in individuals with weakened immune systems.
-
Ingrown Hairs: Ingrown hairs occur when hair grows back into the skin instead of outward, causing inflammation and folliculitis. This is particularly common in individuals with curly or coarse hair.
-
Irritation or Trauma: Friction, excessive sweating, and certain chemicals or irritants can irritate the hair follicles, leading to folliculitis.
-
Weakened Immune System: Individuals with weakened immune systems, such as those with HIV/AIDS or undergoing immunosuppressive therapy, may be more susceptible to developing folliculitis.
-
Personal Items and Environments: Sharing personal items, such as towels, razors, or clothing, can contribute to the spread of bacteria or fungi, increasing the risk of folliculitis. Additionally, exposure to hot tubs, pools, or other water sources with inadequate disinfection can also increase the risk.
Understanding the causes and risk factors associated with folliculitis is essential in preventing its occurrence and managing the condition effectively. By adopting appropriate coping strategies and seeking medical advice when necessary, individuals can alleviate discomfort and promote healing.
Coping with Folliculitis
For individuals dealing with folliculitis, implementing coping strategies can help manage the symptoms and provide relief. Here are some effective approaches to consider:
Good Hygiene Practices
Maintaining good hygiene is essential for managing folliculitis. It’s important to keep the affected areas clean by washing them gently with a mild, non-irritating cleanser. Avoid using harsh soaps or scrubbing vigorously, as these can further irritate the skin. Pat the area dry with a clean towel instead of rubbing, as rubbing can aggravate the condition.
Avoiding Irritants
To prevent exacerbating folliculitis, it’s crucial to avoid irritants that can trigger or worsen the condition. This includes avoiding tight clothing that may rub against the affected areas, as well as avoiding harsh chemicals or irritants that may come into contact with the skin. Opt for loose-fitting, breathable clothing made from natural fibers like cotton.
Applying Warm Compresses
Applying warm compresses to the affected areas can provide soothing relief and help reduce inflammation. Soak a clean washcloth in warm water, wring out the excess, and gently place it on the affected area for 10-15 minutes. Repeat this process a few times a day to help alleviate discomfort and promote healing. Be sure to use a clean washcloth each time to prevent the spread of bacteria.
Using Antibacterial Treatments
In cases where folliculitis is caused by bacterial infection, using antibacterial treatments can be beneficial. Topical antibacterial creams or ointments, as prescribed by a healthcare professional, can help eliminate the bacteria causing the infection. Follow the instructions provided by the healthcare professional and apply the medication to the affected areas as directed.
In addition to these coping strategies, it’s important to remember that folliculitis can have various causes and risk factors. For a comprehensive understanding of folliculitis, including its causes, risk factors, and prevention strategies, please refer to our article on coping with folliculitis.
By incorporating these coping strategies into your routine, you can effectively manage folliculitis and experience relief from the discomfort it may cause. It’s important to note that if symptoms persist or worsen, it is advisable to seek medical advice from a healthcare professional for further evaluation and treatment options.
Soothing Skin Irritation
When dealing with folliculitis, it’s essential to find strategies to soothe and alleviate the skin irritation that often accompanies this condition. Here are some effective coping strategies:
Calming the Itchiness
Folliculitis can be accompanied by intense itchiness, which can further irritate the affected areas. To calm the itchiness, it’s important to avoid scratching, as it can lead to further inflammation and potential infection. Instead, try the following:
- Apply a cool compress or ice pack to the itchy areas to provide temporary relief.
- Use over-the-counter anti-itch creams or lotions containing ingredients like hydrocortisone or calamine.
- Take an oatmeal bath, as oatmeal has soothing properties that can alleviate itching.
Remember, if the itchiness persists or worsens, it’s advisable to consult a healthcare professional for further guidance.
Moisturizing the Affected Areas
Moisturizing the affected areas can help soothe the skin and reduce dryness and irritation. Opt for fragrance-free and non-comedogenic moisturizers to minimize the risk of clogging hair follicles. Apply the moisturizer gently to the affected areas after bathing or whenever the skin feels dry. This can help maintain the skin’s moisture barrier and promote healing.
Avoiding Tight Clothing
Wearing tight clothing can exacerbate folliculitis by causing friction and irritation. Opt for loose-fitting, breathable clothing made from natural fabrics like cotton. This allows for better air circulation and reduces the risk of trapping sweat and bacteria against the skin. By choosing comfortable clothing, you can minimize further irritation and promote healing.
Using Topical Steroids (if prescribed)
In certain cases, healthcare professionals may prescribe topical steroids to help manage the inflammation associated with folliculitis. These steroids can help reduce redness, itching, and swelling. It’s important to follow the prescribed instructions carefully and avoid using these medications for an extended period without medical supervision.
By implementing these coping strategies, individuals with folliculitis can find relief from skin irritation and promote healing. However, it’s important to note that these strategies may provide temporary relief and should be complemented with appropriate medical treatment. If you’re looking for more information on managing folliculitis symptoms, check out our article on managing folliculitis symptoms.
Lifestyle Adjustments
In addition to following proper hygiene practices and using antibacterial treatments, making certain lifestyle adjustments can help manage folliculitis and provide relief from its symptoms. These adjustments include maintaining a healthy diet, managing stress levels, avoiding sharing personal items, and regularly washing bedding and towels.
Maintaining a Healthy Diet
A healthy diet is essential for overall well-being, and it can also play a role in managing folliculitis. Consuming a balanced diet rich in nutrients can support your immune system and promote skin health. Incorporate foods that are high in vitamins, minerals, and antioxidants, such as fruits, vegetables, whole grains, lean proteins, and healthy fats. These nutrients can help strengthen your body’s defense against infections and promote the healing process.
Managing Stress Levels
Stress can potentially affect your immune system and make you more susceptible to infections, including folliculitis. Finding effective ways to manage stress is important in coping with folliculitis. Consider incorporating stress-reducing activities into your daily routine, such as meditation, deep breathing exercises, yoga, or engaging in hobbies you enjoy. It’s also helpful to get enough restful sleep and practice relaxation techniques to promote a sense of calm and well-being.
Avoiding Sharing Personal Items
Folliculitis can be contagious, especially if it is caused by a bacterial or fungal infection. To prevent the spread of folliculitis and minimize the risk of re-infection, it’s important to avoid sharing personal items such as towels, razors, clothing, and hairbrushes. These items can harbor bacteria or fungi that may contribute to the development or worsening of folliculitis. Using disposable items or ensuring proper sanitation of shared items can help reduce the risk of transmission.
Regularly Washing Bedding and Towels
Cleanliness is crucial in managing folliculitis. Regularly washing your bedding and towels can help eliminate any accumulated bacteria or fungi. Use hot water and a mild detergent to ensure proper sanitation. Additionally, avoid using fabric softeners or harsh chemicals that may irritate the skin. If possible, consider using hypoallergenic and fragrance-free laundry products to minimize potential skin irritants.
By incorporating these lifestyle adjustments into your daily routine, you can complement other coping strategies and improve your overall well-being. Remember to consult with a healthcare professional for personalized advice on managing folliculitis and its symptoms. For more information on coping with folliculitis and related topics, refer to our articles on coping with folliculitis and relief for folliculitis.
Seeking Medical Advice
For individuals experiencing folliculitis, seeking medical advice is essential to ensure proper management and relief. Consulting a healthcare professional can provide valuable guidance on when to seek medical attention, available treatment options, and effective prevention strategies.
When to Consult a Healthcare Professional
It is advisable to consult a healthcare professional if:
- The symptoms of folliculitis persist or worsen despite self-care measures.
- The affected area becomes increasingly painful, swollen, or red.
- The condition spreads to other areas of the body.
- You develop a fever along with folliculitis symptoms.
- You have a weakened immune system or a chronic medical condition.
A healthcare professional, such as a dermatologist or primary care physician, can evaluate your condition, provide a proper diagnosis, and recommend appropriate treatment options.
Treatment Options
The specific treatment for folliculitis may vary depending on the severity and underlying cause of the condition. Healthcare professionals may suggest one or more of the following treatment options:
-
Topical Antibacterial Medications: Antibacterial creams, ointments, or lotions may be prescribed to help eliminate the infection causing folliculitis. These medications are typically applied directly to the affected areas.
-
Oral Antibiotics: In more severe cases or when the infection has spread, oral antibiotics may be prescribed to combat the bacterial infection. It is important to take the full course of antibiotics as prescribed, even if symptoms improve.
-
Antifungal Medications: If the folliculitis is caused by a fungal infection, antifungal medications may be recommended to address the underlying cause.
-
Steroid Creams: In certain cases, healthcare professionals may prescribe topical steroid creams to reduce inflammation and soothe the affected areas. However, these should be used with caution and under medical supervision due to potential side effects.
Prevention Strategies
Preventing folliculitis requires adopting good hygiene practices and making certain lifestyle adjustments. Healthcare professionals may provide the following prevention strategies:
-
Proper Hygiene: Maintain good hygiene by regularly cleaning the skin with mild, non-irritating cleansers. Avoid excessive scrubbing or harsh products that can irritate the hair follicles.
-
Avoiding Irritants: Steer clear of irritants, such as tight clothing, harsh chemicals, and irritant cosmetics, that can exacerbate folliculitis symptoms.
-
Regularly Washing Bedding and Towels: Launder bedding, towels, and clothes regularly to minimize the risk of bacterial or fungal contamination.
-
Avoid Sharing Personal Items: Refrain from sharing personal items like towels, razors, or clothing to reduce the likelihood of spreading or contracting infections.
By seeking medical advice, individuals with folliculitis can receive appropriate treatment and guidance on preventive measures. It is important to follow the healthcare professional’s recommendations to effectively manage the condition and minimize the risk of further complications. For more information on coping with folliculitis, visit our article on coping with folliculitis.